Ocular Disease
Million Americans have advanced ARMD
Million Americans have glaucoma
Million Americans are affected by cataracts
At West End Eye Care, we aim to preserve your vision through early detection and intervention of eye conditions using cutting-edge technology. Our thorough eye exams cover every aspect of your eye, allowing us to diagnose various ocular diseases like macular degeneration, glaucoma, cataracts, diabetic retinopathy, uveitis, keratoconus, and more. Schedule your comprehensive examination now to identify any early signs of disease.


Learn More About Common Eye Diseases Below
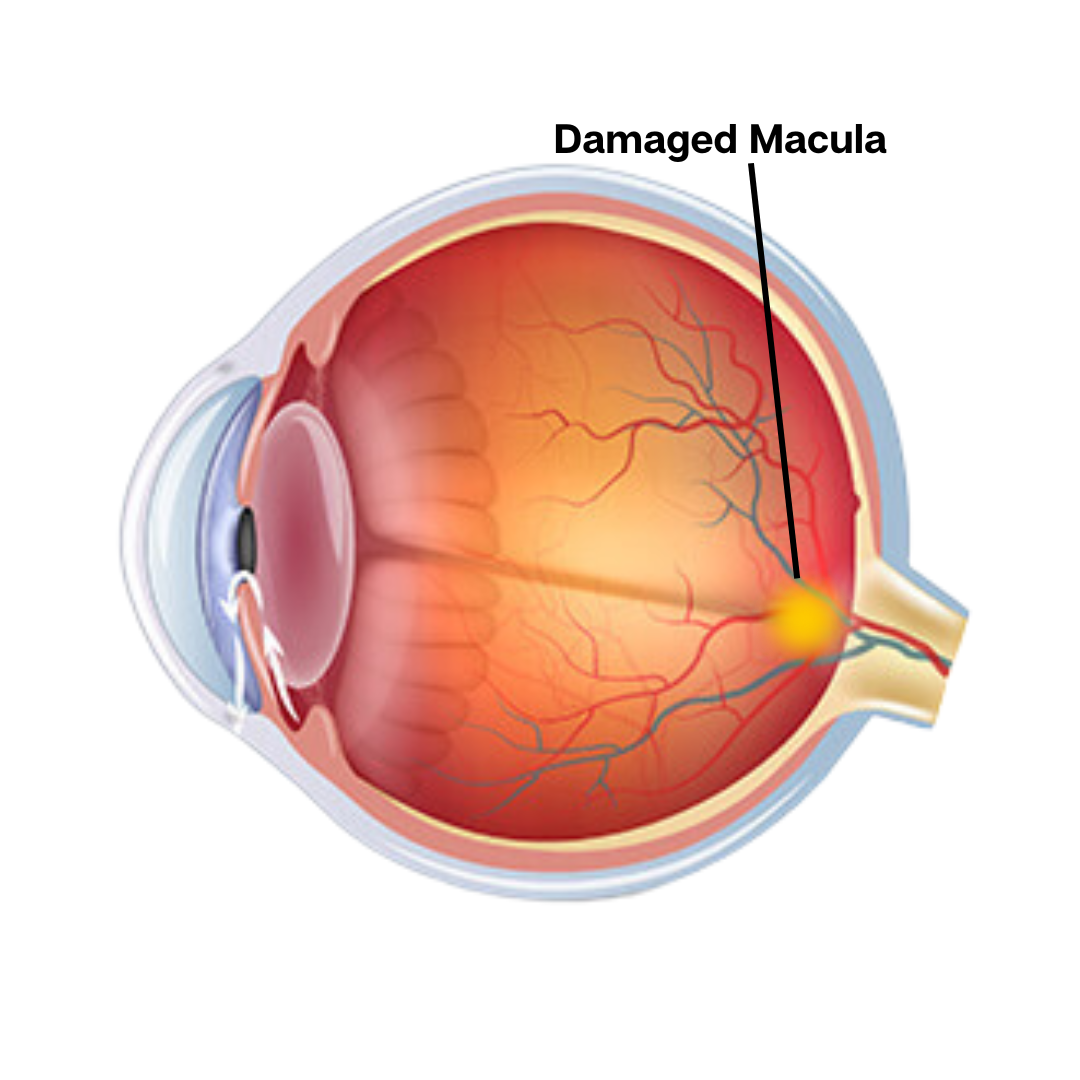
Age-Related Macular Degeneration (ARMD)
A progressive eye condition that affects the macula, the central part of the retina. It can cause central vision loss, making it difficult to see fine details and perform tasks like reading or recognizing faces.
What is ARMD?
ARMD is a disorder characterized by the accumulation of tiny deposits, known as drusen, under the retina’s central part, the macula. Initially, these deposits might not result in any noticeable vision issues. However, as they increase in size and number, they can lead to a blurry or warped central vision. If the retina suffers significant damage due to these deposits, it could start to bleed, resulting in a swift decline in vision.
FAQ's
What is the difference between “Dry” and “Wet” ARMD?
All ARMD begins as the Dry variant, meaning that the drusen deposits are present but the retina is not bleeding. If a specific layer within the retina becomes sufficiently damaged by these drusen, the retina may bleed, a condition we call Wet ARMD. Approximately 10% of dry ARMD cases progress to wet ARMD.
How is ARMD diagnosed?
ARMD is formerly diagnosed when your eye doctor examines your retina and identifies the presence of drusen. Early changes the macula may be more easily detected by an instrument called Optical Coherence Tomography (OCT), which we utilize in our practice.
How is ARMD treated?
Regardless of the type of ARMD, there are a few things we recommend to help lower your risk of vision loss: Lower your blood pressure, wear UV protected sunglasses outside, eat leaf green vegetables daily, and cease smoking. Additionally, a small piece of grid paper calld an Amsler Grid is used to help you identify subtle changes in your central vision at home.
If you have dry ARMD, the most important thing we can do is monitor you closely, watching for signs that wet ARMD has developed. Two large studies called AREDS 1 and 2 have confirmed that taking a specific mixture of vitamins helps to slow down the progression from Dry to Wet AMD. This formulation is available over the counter and should denote that it follows the AREDS-2 Formulation.
If you develop wet ARMD, a medicine in the Anti-VegF family (there are several brand names) is injected into your eye to help clear the blood from the retina. These injections are relatively painless and are often performed several times over the course of months or years to make the bleeding subside. A retina specialist may also use a laser to help stop the bleeding in certain circumstances.
Will I lose my vision if I have ARMD?
Dry AMD often has very little impact on central vision in the early stages of the disease. However, in later stages, central vision is impacted more significantly, causing distorted central vision or a “blind spot” centrally, called a scotoma.
Wet AMD is more likely to have a noticeable impact on central vision, at least prior to treatment. If treatment is administered early on and is successful, vision typically will improve, although not always back to as clear as before it began bleeding.
While it is frightening to consider losing the clarity of your central vision, many take some comfort in knowing that ARMD will never affect their peripheral vision. In other words, although ARMD can affect central vision significantly, it will never cause “black out” blindness where the eye perceives no light.
Why does ARMD occur?
We understand that there are genetic factors that cause ARMD in some but not others. Research into these genetic markers continues. In addition to inherited genes, we know that environmental factors and systemic health plays a role. For example, UV exposure over the course of a lifetime plays a role. We also know that diabetes, hypertension, smoking, and poor diet are risk factors for developing ARMD. Finally, we see ARMD more often in Caucasians, females (although still common in males), and those over 60, hence the name “Age-Related”.
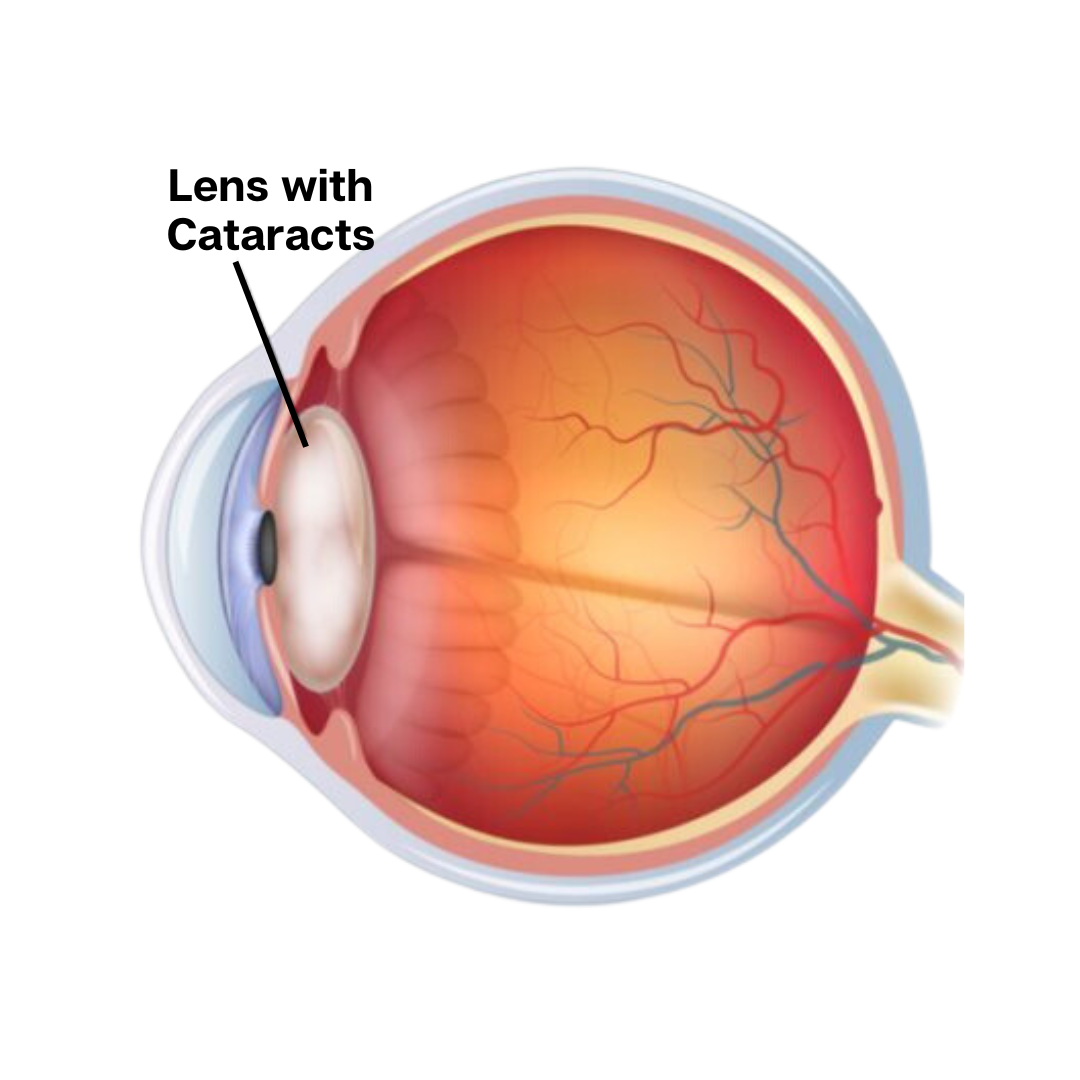
Cataracts
Cataracts are a condition where the lens of the eye becomes progressively opaque, resulting in blurred vision or loss of sight. They typically develop due to aging or other factors like injury, resulting in the clouding of the normally clear lens of the eye.
What are Cataracts?
Cataracts occur when the crystalline lens inside the eye turns from clear to a yellow-brown color or develops other opacities that makes it difficult to see through.
FAQ's
What are the symptoms of cataracts?
As cataracts begin to develop, the most common first symptom involves decreased night vision, including halos and starbursts around lights. As cataracts continue to progress, vision changes include blurred vision, needing additional light to read, and desaturation of colors.
Who gets cataracts?
Cataracts are most commonly age-related, often occuring in the mid to late 60’s and beyond. Other factors, such as diabetes, trauma, or prolonged steroid use can cause premature cataracts to form.
When do I need cataract surgery?
When cataracts begin to interfere with normal tasks that you perform daily, it’s time to have cataract surgery. Each medical insurance has different qualifications that patients must meet before they will pay for the surgery, but these often coincide with the onset of moderate symptoms.
Will I need glasses after cataract surgery?
Cataract surgery is a quick outpatient surgery that often takes around 10 minutes per eye. Surgery is typically performed on one eye with the fellow eye scheduled a few weeks later. Eye drops are used for around a month following surgery to prevent infection and promote healing. While complications can occur, they are not common in routine cataract surgery and are often managed with eye drops alone.
During cataract surgery, the surgeon will remove the natural crystalline lens and replace it with a permanent intraocular lens implant. The benefit of this exchange is that the lens implant can correct your glasses prescription, making most people glasses-free following cataract surgery (many people still need reading glasses after cataract surgery, but may not if the choose a multifocal lens implant).
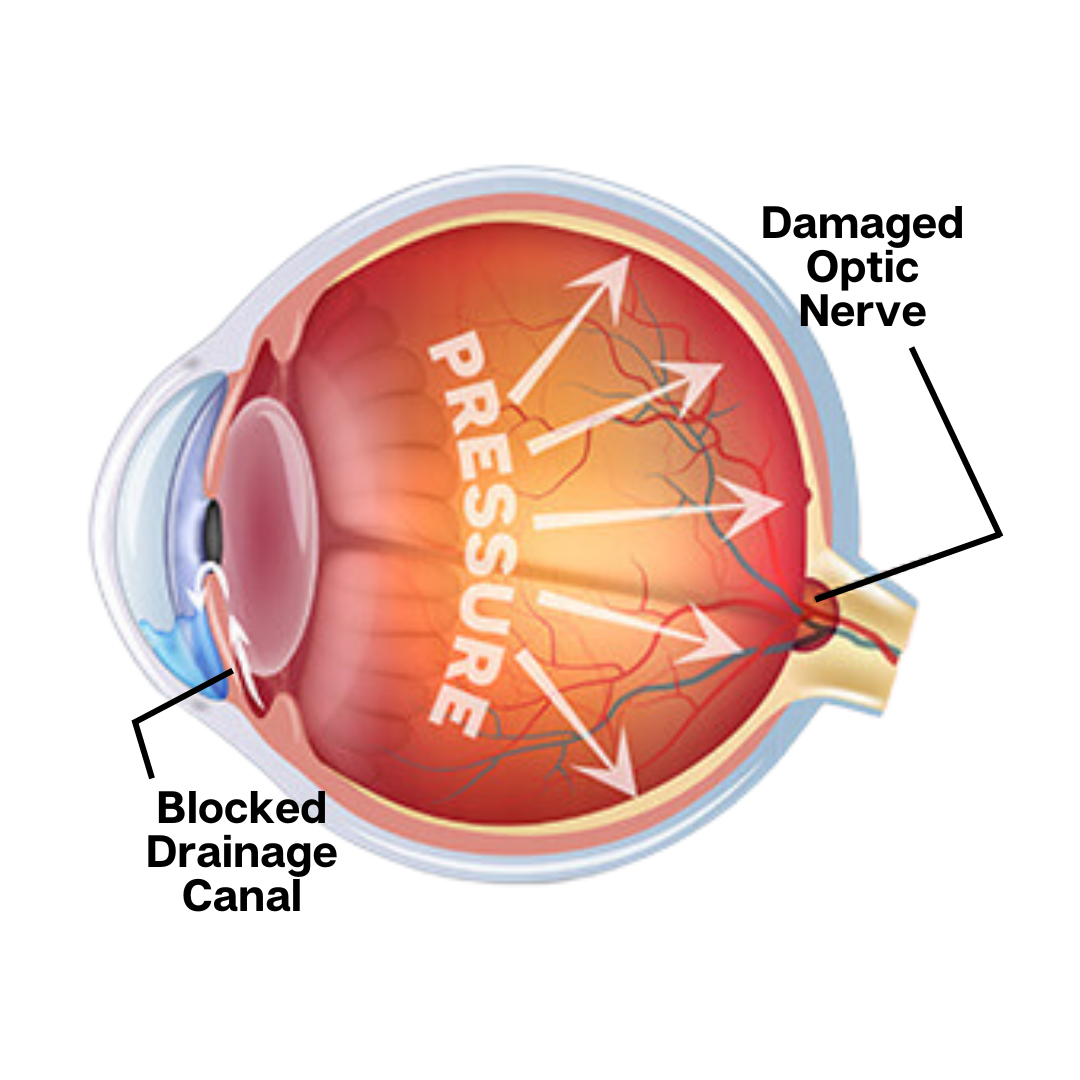
Glaucoma
Glaucoma is a group of eye conditions characterized by damage to the optic nerve, typically caused by unusually high pressure in the eye. If untreated, it can lead to vision loss and blindness.
What is Glaucoma?
Glaucoma refers to a situation where the optic nerve, which transmits the images our eyes see to our brain, undergoes damage because of high intraocular pressure. This damage gradually deteriorates vision and can eventually result in total blindness in the affected eye if not addressed in a timely manner.
FAQ's
What is Intraocular Pressure (IOP) and how high is too high?
A portion of the inside of our eye is filled with a watery substance called aqueous. The aqueous is constantly being pumped into the eye and drained out of the eye. If too much is being produced or not enough is draining out, an excess of aqueous will result, causing increased IOP.
A “normal” IOP usually describes an eye pressure between 8 and 20 millimeters of mercury (mmHg). However, some people have IOP’s higher than 20 and have no discernible damage to their optic nerve. By the same token, some people have IOP’s well below 20, yet still have damage to their optic nerve from that seemingly low pressure. This is why we look at more than just IOP to diagnose glaucoma.
How is IOP measured?
We measure IOP in two ways in our office: the first is called the iCare rebound tonometer which gives us a quick and fairly accurate reading. This is performed on all patients at every exam as a glaucoma screening tool. To measure precise IOP, we us a Goldmann tonometer, which requires instilling a drop of fluorescent yellow drop in your eye prior to measurement. Both methods are quick and painless and give us accurate measurements of IOP.
How is glaucoma diagnosed?
Glaucoma is diagnosed when we can clearly identify damage to the optic nerve in the presence of elevated IOP. The evidence of damage is usually noted on visual field testing, which measures sensitivity of peripheral vision, or on OCT testing, which measures optic nerve thinning.
In some cases, patients have some risk factors for glaucoma (for example, elevated IOP) but no definitive damage to the optic nerve. These patients are labeled “glaucoma suspects” and monitored closely with repeat testing periodically.
How is glaucoma treated?
The primary goal in treating glaucoma is lowering the IOP.This is usually accomplished by using one or more medicated eye drops taken daily. When medication alone does not sufficiently lower IOP, a painless laser procedure called Selective Laser Trabeculoplasty (SLT) is often our next line of treatment.
When eye drops and laser do not suffienctly lower pressure, we typically employ a variety of surgical techniques which are very effective at lowering IOP. Fortunately, the majority of glaucoma patients are successfully treated with medication alone.
What happens if glaucoma is left untreated?
If left untreated, glaucoma will continue to cause irreversible optic nerve damage and vision loss. While patients will not notice early peripheral vision loss, they will eventually develop “tunnel vision” as peripheral vision is progressively lost, and eventually lose all sight in the affected eye.
Am I doing something wrong to make my eye pressure high?
While our eye pressure naturally increases while lying down or when our head is below our heart (ie bending over), these are only temporary. Blood pressure, diet, or stress level have little to no effect on IOP.
